Diagnosis
If liver cancer or hepatocellular carcinoma (HCC) is suspected, the doctor will initiate the necessary examinations. They will help clarify whether a tumor is actually present and, if so, what type of tumor it is and how far it has advanced.
Important steps in detecting HCC are:
- Case history and physical examination
- Ultrasound scan of the liver
- Blood tests
If a tumor is detected in the liver, further examinations will be conducted to determine the type of tumor and the extent of its spread. These examinations include:
- Computed tomography (CT),
- Tissue sampling from the tumor (biopsy),
- Histological examination of the tissue sample,
- magnetic resonance imaging (MRI) when indicated,
- Gastroscopy/colonoscopy if necessary.
The results of all tests must be available to decide on the required treatment steps.
Case history and physical examination
The doctor first records the patient’s current complaints, past medical history, and any risk factors (case history). He then conducts a complete physical examination. This provides important information about the type of disease.
Ultrasound examination
With the aid of an abdominal ultrasound examination, the doctor can see whether the patient has a liver tumor, and, if so, he can pinpoint its location in the organ. Even liver tumors no larger than a few millimeters are detected in many cases. Special types of ultrasound examinations (for example, color-coded duplex ultrasound or contrast-enhanced ultrasound) can provide additional information in individual cases. The ultrasound examination is painless. It can be repeated any number of times, since no harmful radiation exposure is involved. Regular ultrasound examinations (every 6 months) enable early detection of liver cancer in high-risk individuals.
Fig. 3: Ultrasound scan of the liver showing a hepatocellular cancer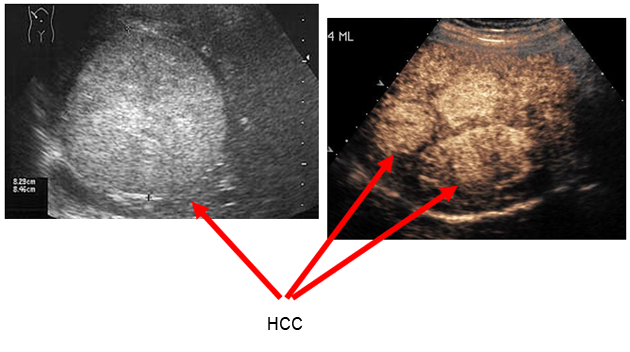
Modified according to Steinberg & Scherübl, Patient Brochure Falkfoundation 2012
Blood tests
Blood tests provide information on the function of organs such as the kidneys, liver, heart and lungs. If liver cancer is suspected, blood is checked for underlying liver disease and for so-called tumor markers. Tumor markers are substances produced in large amounts by tumor cells. Hepatocellular carcinomas often produce the tumor marker alpha1-fetoprotein (AFP), which can be detected in blood.
However, tumor marker levels are not (yet) elevated in many patients with early-stage HCC. On the other hand, elevated AFP levels can also be found in people without tumors. High AFP levels are sometimes found particularly in cases of cirrhosis or chronic hepatitis or during pregnancy. Tumor markers are used primarily to assess tumor growth during treatment and follow-up. Regular ultrasound examinations play a decisive role in the early detection of liver cancer. AFP determination alone, on the other hand, is not very effective for detecting HCC at an early stage in high-risk groups.
Computed tomography (CT) and magnetic resonance imaging (MRI)
Computed tomography or, in some cases, magnetic resonance imaging is used if the ultrasound examination has revealed a lesion or mass in the liver. The two procedures shed light on the location and extension of the tumor as well as on its relationship to adjacent organs. Based on this information, the doctor can decide whether the tumor can be surgically removed and, if so, how extensive the surgery will be. Together with ultrasound, both these procedures are highly accurate in distinguishing between benign and malignant liver tumors.
Computed tomography (CT) is a specialized x-ray procedure for examining the body layer-by-layer. It produces cross-sectional images of organs. A CT scan of the chest and abdomen is performed in order to determine whether the liver cancer has spread to other organs.
Magnetic resonance imaging (MRI) also enables layer-by-layer examination of organs. This procedure uses magnetic fields, not x-rays.
The doctor decides on a case-by-case basis whether to use computed tomography or magnetic resonance imaging. In either case, a contrast medium is injected into a vein in order to enhance tumor visibility during the CT or MRI. The examinations are painless.
Fig. 4 and 5: CT- and MRI-images of HCCs.
The hepatocellular cancer is marked by yellow arrows.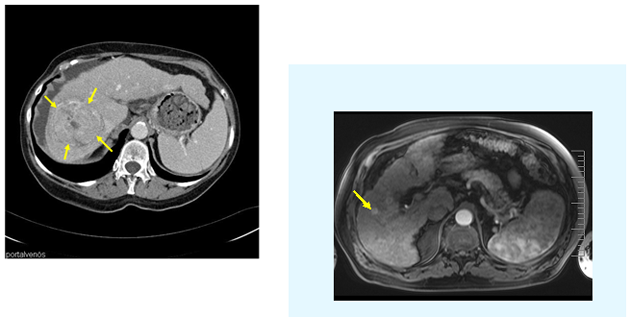
Modified according to Steinberg & Scherübl, Patient Brochure Falkfoundation 2012
Chest x-rays
Chest x-rays are performed to check the condition of the heart and lungs. They also enable the detection of lung metastases.
Biopsy
The diagnosis of liver cancer can often only be definitely confirmed by histological examination of tumor tissue under the microscope. Prior to treatment, the doctor therefore takes a tissue sample from the tumor by puncture (biopsy). To obtain the sample, tissue is removed from the suspicious area with a fine needle under CT guidance and then examined. The abdominal wall is punctured from the outside under local anesthesia so that the patient feels no pain.
The tissue sample is then histologically examined by the pathologist. This enables a distinction to be made between benign and malignant lesions as well as between liver cancers and liver metastases (from other tumors).
Puncture is not necessary if a definite diagnosis has already been made on the basis of the history, ultrasound, computed tomography and tumor marker determination (AFP).
Endoscopy of the stomach (gastroscopy) and of large bowel (colonoscopy)
A liver tumor suspected of being a “secondary” tumor (a metastasis from a tumor outside the liver) will require a gastroscopy and colonoscopy. Stomach and bowel cancer often tend to metastasize to the liver. In addition, a gastroscopy is generally advisable in all new cases of liver cancer in order to detect esophageal or gastric varices and to define their risk of bleeding.
To perform a gastroscopy or colonoscopy, the doctor inserts a tube, a so-called endoscope, into the patient’s stomach or large bowel. The endoscope is a flexible finger-thick instrument equipped with a light and a small video camera. It enables the doctor to look inside the organs on a monitor and to take tissue samples if necessary. The tissue samples are then examined under the microscope for cancer cells. Nowadays, a gastroscopy or colonoscopy is performed under short-term anesthesia so that the patient sleeps during the examination.
Fig. 6: Esophagogastroduodenoscopy (= Endoscopy of the gullet, stomach and duodenum): Varices of the gullet are detected.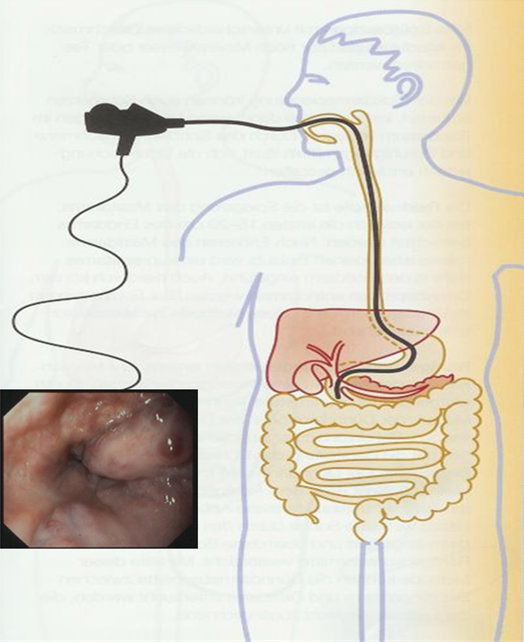
Modified according to Steinberg & Scherübl, Patient Brochure Falkfoundation 2012
Contact
Center of Interventional Hepatobiliary Medicine
Prof. Dr. med. Hans Scherübl
Vivantes Klinikum Am Urban
Academic Teaching Hospital of Charité, Berlin
Dieffenbachstraße 1
10967 Berlin
Tel: + 49 30 130 225201
Fax: + 49 30 130 225205
Email: This email address is being protected from spambots. You need JavaScript enabled to view it.
vivantes.de/kau/gastro/
